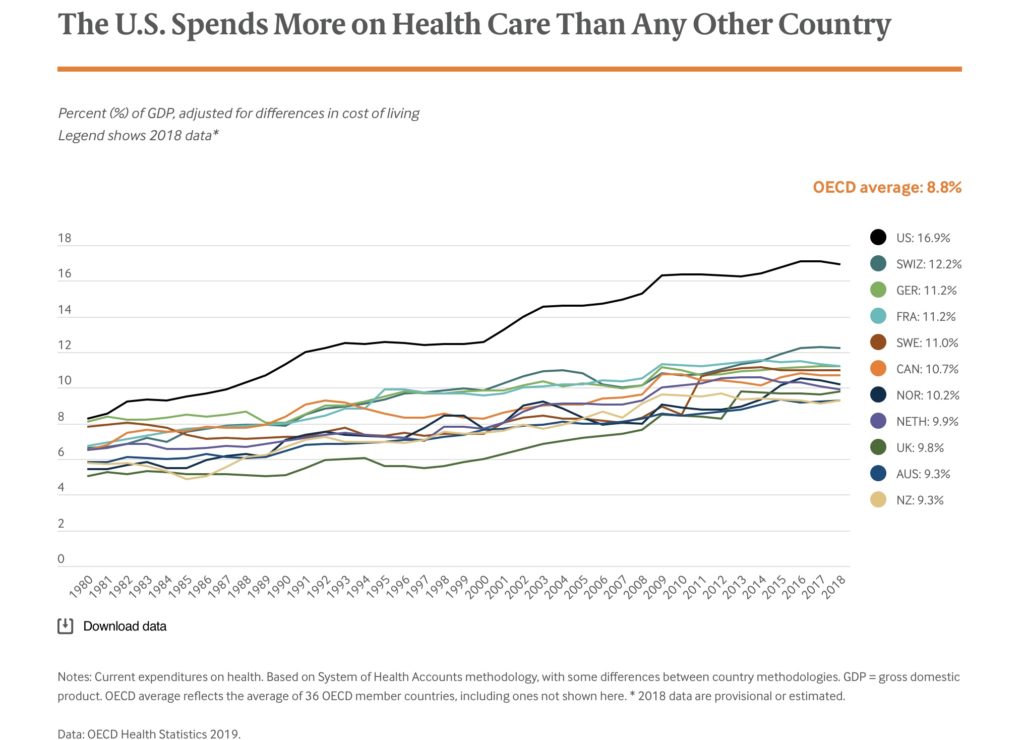
The average person in the US spends more than $16,000 per year (2019) on healthcare. Although we utilize healthcare services at the same rate as the other high-income countries, we spend about twice as much per person as the other industrialized countries, see graph above. For details: https://www.commonwealthfund.org/publications/issue-briefs/2020/jan/us-health-care-global-perspective-2019
Together, physicians and hospital expenditures account for a bit more than half of US healthcare spending. Some of the excessive expenditures can be attributed to the fact that services provided by physicians and hospitals are reimbursed at about twice the rate seen in the other high-income countries.
Physicians are acutely aware that the cost of healthcare is a problem for their patients. When we recommend a new procedure/medicine/treatment plan, we know that many patients are counting the dollars they are going to be required to spend, even though the vast majority of patients say nothing to their physician. I spend a lot of time during my office visit trying to understand if the patient will be able to afford my suggested treatment and whether the patient will even tell me when they can no longer afford to take their medicines. The Commonwealth Fund has shown that 35-40% of patients do not obtain recommended healthcare services because of the high cost of healthcare.
There are four clinical situations which can be particularly financial injurious to a patient. The common thread in all of these scenarios is that the patient has a clinical event which required them to obtain healthcare from a provider with whom they have no pre-existing contractural relationship. For example, the patient has:
-
- no insurance
- poor quality insurance
- there was a bureaucratic “referral problem”
- they received care from an “out-of-network” provider
Hospitals, physicians and other healthcare providers usually do not know what they are going to get paid for any given service, as they have contracts with many insurance companies, each with its own payment rate. In an attempt to capture all potential revenue, healthcare providers and institutions create an egregious fee schedule which is set at several multiples of what they expect to get paid from the most lucrative payer. This fee schedule is neither reflective of a competitive marketplace nor derived from the actual cost of the services provided.
When a patient obtains care from an institution or healthcare provider with whom they have no pre-existing contractural relationship, the provider is an “out-of-network” provider who may legally charge the patient any fee they wish, even if it is egregious and economically irrational.
Many patients are occasionally forced to obtain care from an out-of-network provider or institution. This will occur when a patient has a medical emergency and they must seek care from the nearest provider, even if they are out-of-network. It can also happen when a patient is admitted to an in-network hospital but a treating physician, such as a radiologist or pathologist, who provides services to the patient behind the scenes is an out-of-network provider. Thus, even patients who are fully insured, and through no fault of their own, may be forced to obtain healthcare services from an out-of-network provider. They then are then legally responsible to pay an egregious medical bill.
For more than several decades we have tried innumerable interventions to reduce healthcare spending. Unfortunately none have had a durable and significant impact. The latest theory is that if healthcare providers/institutions simply published their prices, the cost of healthcare would come down. To date, objective data has shown that “transparency in pricing” does not work.
We must protect patients from egregious medical fees and this could be accomplished if we legally capped the maximum allowed billing fee healthcare providers and institutions can charge a patient. I would suggest that we begin by capping billing fees at 250% of Medicare allowed billing.
Based on the Congressional Budget Report (https://www.cbo.gov/system/files/115th-congress-2017-2018/workingpaper/53441-workingpaper.pdf and as shown in the above graph) this very generous upper limit cap on medical fees would marginally impact only a very tiny fraction of all healthcare providers and institutions while simultaneously protecting all patients, insured and uninsured, from receiving a medical bill which is objectively irrational and potentially financially incapacitating.
Once this system is in place and health economist have had a chance to assess its effectiveness, then, if it is found to be effective, the 250% upper limit could be serially decreased so that we create a healthcare system that our society can afford.
As our healthcare system is not fiscally sustainable, it has to change. This proposed cap on the fee schedule of healthcare providers and institutions is a reasonable place to begin.
Hayward Zwerling, M.D.
10/19/2019