This article was originally posted on The Healthcare Blog in May 2019. This version has been slightly updated.
The high cost, low quality and systemic inequities of the U.S. healthcare system have been the impetus for its redesign. Our healthcare system is now controlled by Consolidated Healthcare institutions, Insurance companies, Pharmaceutical companies and Health Information Technology companies (CHIPHIT complex). The CHIPHIT complex, along with the Federal Government, will create and control our future healthcare system. Ominously missing from this list are independent healthcare policy experts, independent healthcare providers and members of the general public.
Historical precedents have demonstrated that the CHIPHIT complex is incapable of creating the healthcare system we need.
Thus, if we hope to build a low cost, high quality, egalitarian healthcare system, physicians and their professional organizations must take an emphatic stand against the CHIPHIT complex today.
Consolidated Healthcare Institutions
There are innumerable mandates which make running a small medical practice very difficult. As a result, many younger physicians will no longer attempt to start a new medical practice and existing profitable practices, which are looking to off- load their regulatory burdens, are being acquired by large healthcare institutions and private equity firms.
While these consolidated healthcare institutions vocalize their desire to improve our healthcare system, many enforce a uniformity on the practice environment which belies the reality of patient care; that there is no “best” practice model, nor are there information technology tools which work well for all physicians. This imposed uniformity stifles physician innovation, which is a necessary precondition to improve our healthcare system.
If the consolidated healthcare institutions want to maximize the probability of improving our healthcare system, they should encourage their physicians to innovate, they must abandon their drive toward practice uniformity and they need to defer all practice related decisions, including the selection and design of information technology tools, to the professional judgment of the relevant healthcare providers.
Insurance Companies
Health Insurance companies tell their patients which primary care physician and specialists they may consult. For many patients, lifetime continuity of care is no longer possible and is a cause for anxiety for some elderly and chronically ill patients.
Insurance companies tell physicians which tests they may order and which medications they may prescribe. As a result of the restrictive formularies, physicians are not infrequently required to use an “approved” medication even if they believe the patient would be better served with a non-formulary alternative. While it is possible to “appeal” for an exemption, many physicians have been so beaten down by serial and irrational denials that they have changed their practice patterns against their own professional judgement.
Several years ago I needed to obtain an emergency head CT scan for a patient who had “the worse headache of my life.” As the CT required a “prior approval,” I called the insurance company and was told the CT was “not indicated.” I explain to the insurance company representative (who lacked the clinical training to make such a decision) that if the insurance company did not approve the CT scan, I would send the patient to the ER where the insurance company will incur both the cost of an ER visit and the cost of an emergent head CT scan. The insurance company representative said, “OK, order the CT scan and if it is abnormal we will pay for it.” One can only experience events like this so many times before one becomes disillusioned and reluctant to engage with insurance companies.
While many have assumed that some health insurance companies have prioritized their own financial bottom line ahead of the healthcare needs and fiduciary obligations to their patients, this illegal business model was definitively illuminated by Judge Spero’s ruling in Wit v. United Behavioral Health.
Pharmaceutical Companies and Pharmacy Benefit Managers
The pharmaceutical industry has blocked the expiration of patents on brand-name medications thus delaying the creation of inexpensive generics.
They have used legal loop-holes to acquire inexpensive generics and turned them into non-generics, which allows them to increase the price orders of magnitude. URL Pharma converted colchicine to a non-generic medication and then increased the price by more than 5,000%.
The pharmacy benefit managers (PBM) aggregate the purchasing power of multiple insurance companies giving them the market strength to (theoretically) lower drug prices. Nevertheless, the cost of medications continue to increase faster than the rate of inflation and health policy experts have begun to implicate the PBMs as a contributing factor to the high cost of pharmaceutical agents. For example, the price of a vial of Lantus insulin has increased 300% in the last decade despite the fact that it is exactly the same medicine which is being sold in the same container.
Health Information Technology Companies
The electronic health record (EHR) vendors have inserted themselves in the middle of the exam room and now have an inappropriate amount of influence on the interaction between a patient and their physician. In the exam room, physicians have to “click” on clinically irrelevant buttons in the EHR. The poor design of EHRs force physicians to spend two hours entering data into the EHR, much of it clinically irrelevant, for every hour of face-to-face patient care, a massively inappropriate use of a physician’s skill set.
While there have been successful EHR implementations, sadly, that is not universally the case. EHRs do have an important role in our health care system but they are not the panacea the EHR vendors claim. They are simply one tool of many which can help physicians, if properly designed, to provide care to their patients.
As a result of my decades long experience creating an EHR, I am certain that EHRs would be far more useful to physicians if the person who has the ultimate authority over all EHR design/implementation decisions:
- is required to use the EHR on a daily basis
- has deep knowledge about clinical medicine
- has some experience in computer programming
- has an in-depth understanding about information technology and
- is committed to evidence based medicine while acknowledging its limitations.
Physician Burnout
The accumulation of the aforementioned assaults on the physician’s professional judgement has resulted in “physician burnout,” which is “a long-term stress reaction characterized by depersonalization, including cynical or negative attitudes toward patients, emotional exhaustion, a feeling of decreased personal achievement and a lack of empathy for patients.” It is a prime cause of physicians prematurely ending their clinical careers, reduces the quality of healthcare provided and increases patient mortality. I know several physicians who had previously committed large amounts of time trying to improve their healthcare system but have since withdrawn their involvement because “nothing ever changes.”
Dangers of the CHIPHIT Complex
The CHIPHIT complex, in conjunction with the Federal Government, have created a healthcare system which undervalues direct patient care and overvalues clinically irrelevant documentation. They institute roadblocks which thwart physician innovation and adversely impact our ability to provide healthcare. They are the cause of physician burnout and the reason many physicians, nurses, pharmacists and CMOs (personal anecdote) are dissatisfied with the current design of our healthcare system.
In President Eisenhower’s farewell address, he said “We must guard against the acquisition of unwarranted influence … by the military-industrial complex…” The U.S. healthcare system rivals the size of the military-industrial complex and the CHIPHIT complex already has an inappropriate amount of influence over our healthcare system. If we choose to ignore this precedent, our healthcare system will continue to be dominated by the CHIPHIT complex for many decades into the future and that will prevent us from obtaining the healthcare system we need.
The primary goal of the CHIPHIT complex is to maximize their revenue, as it should be in a free market economy. If we want their primary goal to be the optimization of our healthcare system then the laws which govern the CHIPHIT complex must be changed – an unlikely outcome in today’s political climate.
As the CHIPHIT complex is incapable of building the healthcare system we need, we must look beyond the CHIPHIT complex for a mechanism to repair our defective healthcare system.
A Potential (Partial) Solution
Fortunately, there is objective data which shows us how to solve some of our healthcare system’s failures. As was discussed in the 2014 Robert Wood Johnson Foundation report “Time to Act: Investing in the Health of Our Children and Communities,” “The key to better health does not lie primarily in more effective health care.”
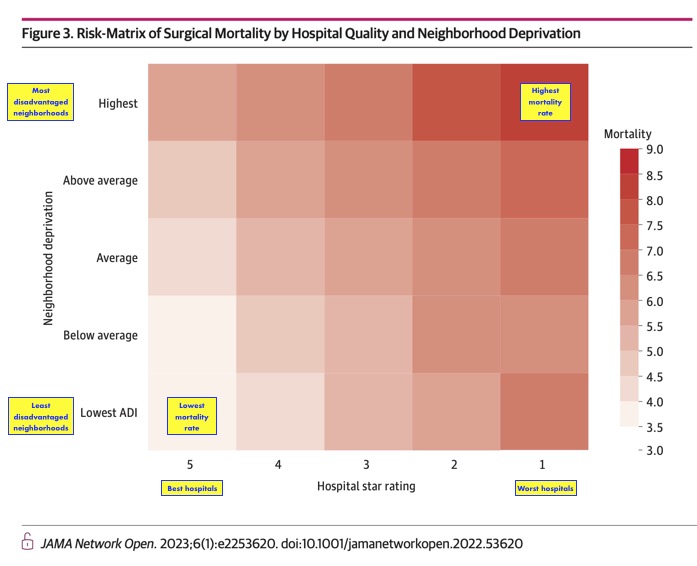
If we hope to improve the health of Americans then we must address issues that are outside the walls of our hospitals’ and physicians’ offices so as to reduce the inequities which are a major determinate of a person’s healthcare statistics as low socioeconomic status alone increases hospital mortality even in the best hospitals.
If we hope to improve the health of all Americans we must redirect funding away from the CHIPHIT complex and toward entities that prioritize a high quality, low cost, egalitarian healthcare system.
We must invest in our youth, in those who are educationally, socially and economically disadvantaged. In doing so we will reduce the prevalence of obesity, cigarette use, other unhealthy behaviors and societal inequities which disproportionately afflict segments of our society and drive up healthcare and avoidable social expenditures. This model of healthcare has already been implemented in other countries and is objectively more effective and efficient than our current healthcare system.
Hayward Zwerling, M.D.
5/8/2019
Addendum of 10/11/2022: As a consequence of the above, see My Retirement Letter to My Patients and Hiking the Alaskan Wilderness Induced a Moment of Cognitive Clarity
Addendum 2/3/2023: Revised final section adding some recently published data.
